Our Story
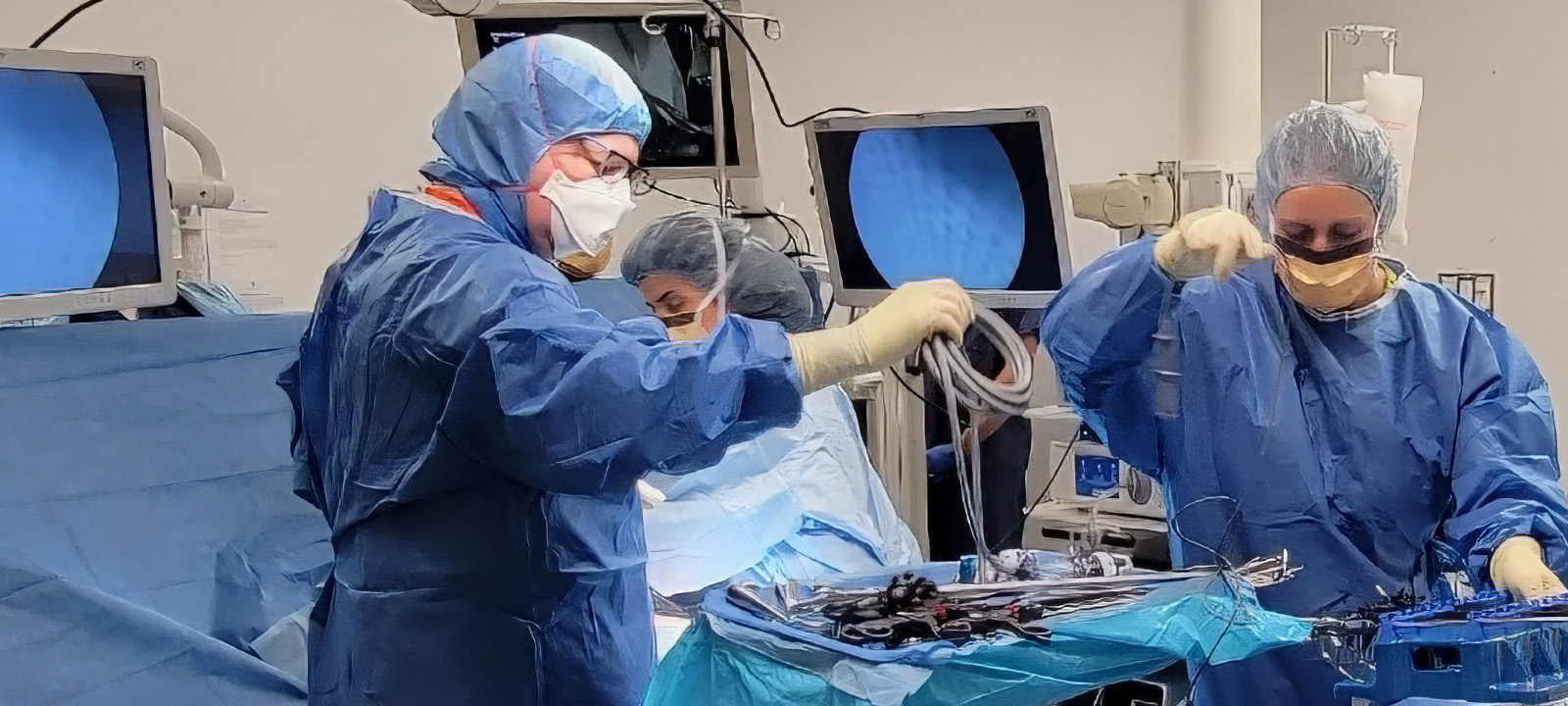
Dr. Gagner and Surgical Innovation
Michel Gagner, MD, born in Montreal, Quebec, Canada, completed his residency in general surgery at McGill University and undertook a fellowship in Paris in liver surgery and a second fellowship at the Lahey Clinic (MA) in pancreatic and complex gastrointestinal (GI) surgery. He was an early practitioner of laparoscopic technique (world’s first laparoscopic removal of adrenal glands, liver, bile duct, and pancreas). He was also a pioneer in endoscopic surgery (treatment of parathyroid and thyroid tumors); robotic technique; and, with Professors Marescaux and Leroy in Strasbourg, telesurgery (first transatlantic robot-assisted surgery). Dr. Gagner (Cleveland Clinic, Mt. Sinai School of Medicine, Cornell University, Université de Montréal, Florida International University) is currently Director and Chief of Surgery at his private clinic, Westmount Square Surgical Center, in Montreal, where he concentrates on metabolic/bariatric surgery (MBS) for weight loss and treatment of type 2 diabetes.
LSG has demonstrated effective short- and medium-term weight loss and resolution of associated medical conditions while maintaining normal GI continuity and introducing no anastomoses. LSG can be safely revised, and may be used to revise other MBS procedures. Between 2016–2020, LSG overtook all other MBS operations in global prevalence (50.2%).4,5
Dr. Gagner is the author or co-author of over 544 works, including peer-reviewed articles and chapters and 11 books, the most recent of which is devoted to this evolving field, Magnetic Surgery (Springer, Aug., 2021). In 2016, he received the Surgical Innovation Award from the American Society for Metabolic and Bariatric Surgery (ASMBS). He also holds patents for new methods to treat obesity and develop GI anastomoses. As a young attending surgeon, fashioning a full-thickness anastomosis — an essential functional element of many GI, vascular, and other procedures — became a key minimally invasive surgery (MIS) objective for him. Compression anastomosis technique was an emerging option using the biodegradable anastomotic ring (BAR) (Valtrac, American Cyanamid). However, at that time, Dr. Leon Hirsch led US Surgical Corporation in the invention of widely successful laparoscopic stapling, delaying development of the compression approach.
Next-stage MIS — Magnetic Compression
By engaging the compressive force of two elongated magnets aligned across two GI segments, a tunnel is created gradually between them and collagen is deposited around the magnets’ edges. An anastomosis is formed at 7-21 days, and the magnets are expelled naturally.6,8 The goal is that by utilizing this natural process, fewer acute leaks, infections, strictures, and ulcerations will occur.

Dr. Gagner coined the novel methodology “delayed anastomosis technology” (DAT). The unhurried DAT approach is highly efficient. The intent of the approach is to increase safety intraoperatively and postoperatively, require less anesthesia, less time in hospital, and fewer rehospitalizations for complications. DAT will facilitate staging of complex operations into two or more brief outpatient procedures with the intent to further reduce morbidity and mortality.
Building a Novel Magnetic Surgery Company
After reconnecting at ASMBS in 2019, Dr. Gagner and Thierry Thaure, a medtech entrepreneur with experience at Cephea Valve Technologies / Abbott, Intuitive Surgical, Accuray, Origin Medsystem, EndoGastric Solutions, Guidant, founded GT Metabolic (Silicon Valley, CA) in May 2020, incorporating Dr. Gagner’s intellectual property (IP). Mr. Thaure serves as Chief Executive Officer and Dr. Gagner as Chief Medical Officer.
Together, Mr. Thaure and Dr. Gagner are working to lay the foundation to make a meaningful impact on the future of bariatric surgery and metabolic surgery with the innovative MIS magnetic DAT products and procedures. Currently, patients are being enrolled in five centers across Canada and Europe. Patients have undergone initial GT clinical trials, including the first-in-human (FIH) and proof-of-concept studies. The first-general multi-center clinical trial evaluating side-to-side DI anastomosis with or without LSG using the Magnetic Anastomosis System (Magnet System) supported De Novo marketing authorization by the US Food & Drug Association (FDA).6-8
- “Duodenal Switch May Be More Effective than Gastric Bypass, NewYork-Presbyterian/Weill Cornell Study Finds: NYP.” NewYork-Presbyterian, 14 Oct. 2005, www.nyp.org/news/duodenal-switch-may-be-more-effective-than-gastric-bypass.
- Noel, P., Nocca, D. (2020). The Future of Sleeve Gastrectomy. In: Gagner, M., Cardoso, A., Palermo, M., Noel, P., Nocca, D. (eds) The Perfect Sleeve Gastrectomy. Springer, Cham. https://doi.org/10.1007/978-3-030-28936-2_38.
- Zundel, N., Hernandez R., J.D., Gagner, M. (2020). Laparoscopic Sleeve Gastrectomy: Technique and Outcomes. In: Nguyen, N., Brethauer, S., Morton, J., Ponce, J., Rosenthal, R. (eds) The ASMBS Textbook of Bariatric Surgery. Springer, Cham. https://doi.org/10.1007/978-3-030-27021-6_13.
- Brown W, Kow L, Shikora S, et al. Sixth IFSO Global Registry Report 2021. Henley-on-Thames: IFSO & Dendrite Clinical Systems Ltd; 2021. Available at: https://www.e-dendrite.com/IFSO6.
- Angrisani L, Santonicola A, Iovino P, Vitiello A, Higa K, Himpens J, Buchwald H, Scopinaro N. IFSO Worldwide Survey 2016: primary, endoluminal, and revisional procedures. Obes Surg. 2018;28:3783–94.
- Gagner, M., Almutlaq, L., Cadiere, G.-B., Torres, A. J., Sanchez-Pernaute, A., Buchwald, J. N., & Abuladze, D. (2023). Side-to-side magnetic duodeno-ileostomy in adults with severe obesity with or without type 2 diabetes: Early outcomes with prior or concurrent sleeve gastrectomy. Surgery for Obesity and Related Diseases. https://doi.org/10.1016/j.soard.2023.10.018.
- Gagner, M., Abuladze, D., Koiava, L. et al. First-in-Human Side-to-Side Magnetic Compression Duodeno-ileostomy with the Magnet Anastomosis System. OBES SURG 33, 2282–2292 (2023). https://doi.org/10.1007/s11695-023-06708-x.
- De Novo marketing authorization DEN240013. MagDI™ System for side-to-side duodeno-ileal anastomosis granted De Novo marketing authorization from the U.S. Food and Drug Administration (FDA). 2 July 2024.
